ANS Tutorial
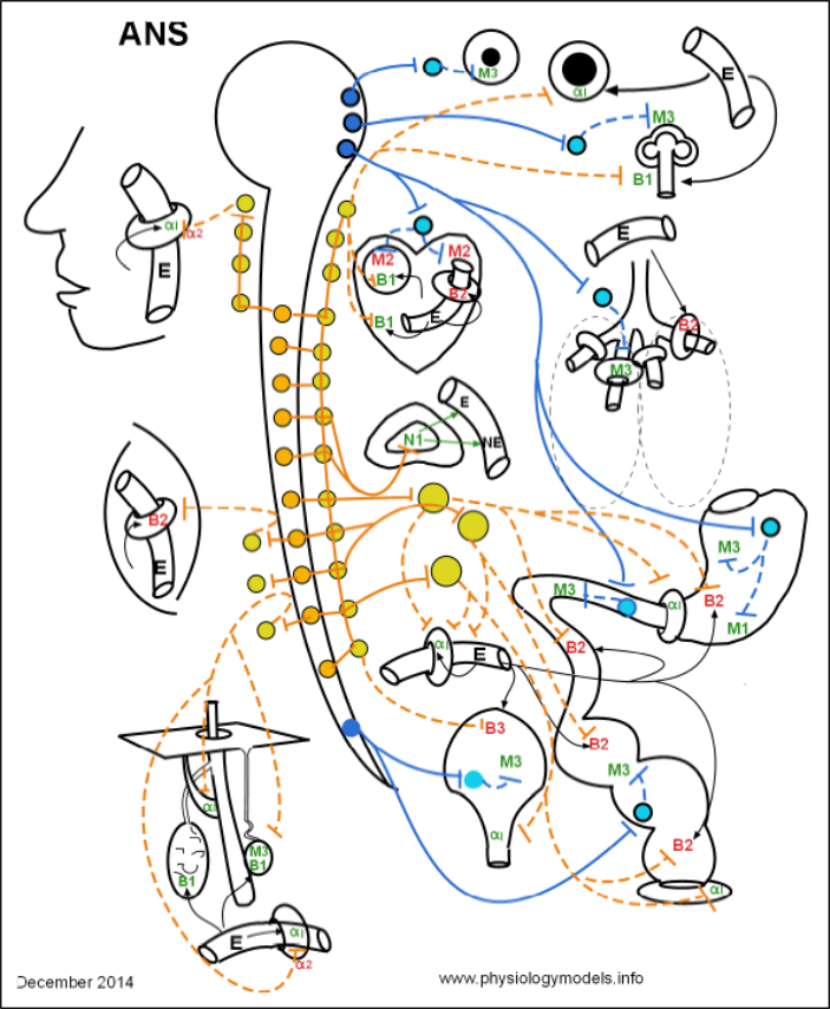
Click on 'Model' in the menu to the left to view this at any time. The model depicts the interrelationships between the major topics of this tutorial.
Click on "Design" in the Menu to the left.
You can select and print a copy from this page.
Overview
The activities of your internal organs are simultaneously controlled by two sets of nerves; one increases the activity of the organ while the other ... simultaneously ... decreases that activity. The end result depends on which nerve dominates at that moment in time.
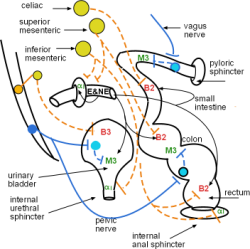
These nerves comprise the two divisions of the autonomic nervous system (ANS). Anatomically, they are distinguished by where they exit the central nervous system. Nerves exiting the brain and sacral spinal cord (blue in the above model) are collectively known as the "carnio-sacral outflow" or the parasympathetic division (PSNS). Nerves exiting other sections of the spinal cord (orange in the model) are known as the "thoraco-lumbar outflow" or the sympathetic division (SNS). Notice, in the model, that there are no nerves exiting the cervical region of the cord.
The ANS is the involuntary portion of the nervous system. Its nerves begin within the central nervous system and connect with target organs via two-neuron pathways. Nerves in the ANS are totally efferent with impulses traveling from the central nervous system ending in target organs throughout the body. The cells within these organs have surface membrane receptors to which neurotransmitters, released by the nerves, attach. These cells are either smooth muscle cells, cardiac pacemaker cells, cardiac muscle cells or glandular cells. Smooth muscle cells respond by either increasing or decreasing their muscle tone, the cardiac pacemaker increases or decreases the heart rate, the cardiac muscle contracts more or less strongly with each beat and glands increase or decrease their secretions.
The major point to always keep in mind is that most-- but not all -- organs are responding to neurotransmitters of both divisions simultaneously.
Scroll down for a description of the model's design.
Design of the Model
As you read through each section below, scroll back up to this illustration
and locate the part
of the model being described. Better yet, if you are at a computer open a new tab to this site and click on
'Model' to open up a full-size image of the illustration and show this as a second side-by-side screen.
Central Nervous System (CNS)
The large open circle with a long hollow tail running the length of the model represents the brain and spinal cord.
Nerves & Ganglia
Nerves of the autonomic nervous system contain numerous, parallel, two-neuron chains. The cell body of the first neuron in each chain lies within the CNS; its cell body is drawn as a small dark-blue or orange circle and its axon is represented by a solid colored line extending from it. The second neuron in each chain lies outside of the CNS and is drawn as a small light-blue or yellow circle with a dashed colored line extending from it.
Each nerve consist of hundreds of individual neurons. When wrapped in connective tissue an obvious bulge is formed where the cell bodies of the second neurons are grouped together. Such a bulge is called a ganglion. It is for this reason that the first neurons in the chain are described as "preganglionic" and the second neurons as "postganglionic."
In the model, the light-blue and yellow circles outside the central nervous system can be interpreted as representing either the a postganglionic cell body or a ganglion. Similar circles drawn inside the brain and spinal cord (dark-blue and orange) can represent either preganglionic cell bodies or clustered cell bodies of preganglionic neurons. In the brain such clusters are called nuclei and in the spinal cord they are referred to as lateral grey horns.
Heart
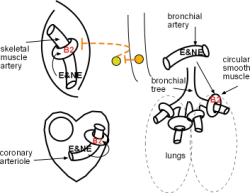
The thorax houses the heart drawn to the right of the upper spinal cord. The circle inside the heart is the pacemaker. The tubular structure inside the heart represents small coronary arterioles.
Respiratory Organs
The branching structure to the right of the heart represents the bronchial tree. The donut-shaped structures around the branches are the bronchial muscles that regulate the diameter of the airways. The tubular structure above the lungs represents the bronchial arteries.
Gastrointestinal Tract
In the lower right quadrant of the model is the GI tract. Shown here are the stomach, pyloric sphincter, small and large intestines and internal anal sphincter. The tubular structure to the left of the small intestine represents splanchnic arteries that supply these organs. The arrows leaving it represent epinephrine (E) and norepinephrine (NE) diffusing to these organs.
Excretory System
The urinary bladder and its internal urethral sphincter are shown below the splanchnic artery and to the left of the large intestine.
Adrenal Gland
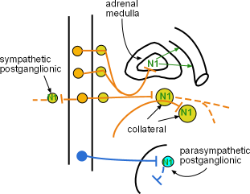
An adrenal gland is shown just beneath the heart. Its central portion is the medulla which releases the hormones epinephrine (E) and norepinephrine (NE) into the capillaries (shown to the right) that pass through the gland.
Arteries
Arteries are shown throughout the model as small curved tubes encircled by a donut. The donut represents vascular smooth muscle that encircles resistance arteries. When these muscles contract the diameter of the vessel narrows and reduces blood flow; when they are relaxed the pressure of the blood causes the vessel diameter to enlarge and flow to increase.
Structures in the Head
A facial profile containing a blood vessel that supplies the linings (mucosae) of the nose (nasal) and mouth (oral) is shown in the upper-left corner. At the top-center of the model are two illustrations of the iris of the eye showing the pupil constricted and dilated. Just below and to the right of the dilated pupil is a representation of the functional unit of salivary glands.
Organs Located in the Skin
Illustrations at the lower left of the model depict structures found in the skin. The oval structure to the left is an apocrine sweat gland entering the hair follicle. These are most abundant in the armpits and groin area. The structure running from the follicle to the lower surface of the skin is the arrector pili muscle. The smaller oval structure to the right of the follicle is an eccrine sweat gland. This is the 'normal sweat' that evaporates to cool the body. Below these structures is a dermal artery.
Skeletal Muscle Arteries
The spindle-shaped structure at center left represents the skeletal muscles. The tubular structure within it represents arteries.
Parasympathetic Division / Cranio-sacral Outflow
Nerve Anatomy
Inspection of the entire model shows "blue nerves" exiting the central nervous system from the brain and sacral spinal cord -- thus the name cranio-sacral outflow. It is also called the parasympathetic division because its activity is auxillary to the sympathetic division. The anatomy of this division is much simpler than the sympathetic division that is represented by "orange nerves" in the model.
Throughout the model the preganglionic cell bodies (dark-blue circles) give rise to axons (solid blue lines) that extend toward their targets and end as neurosecretory terminals (blue bars) that secrete acetylcholine. Most targets are postganglionic neurons; however, note that the adrenal medulla has no PSNS innervation. The postganglionic cell bodies (light blue circles) lie close to, or within, the target organs. Their axons (dashed blue line) are relatively short and end in terminals (blue bars) that secrete acetylcholine.
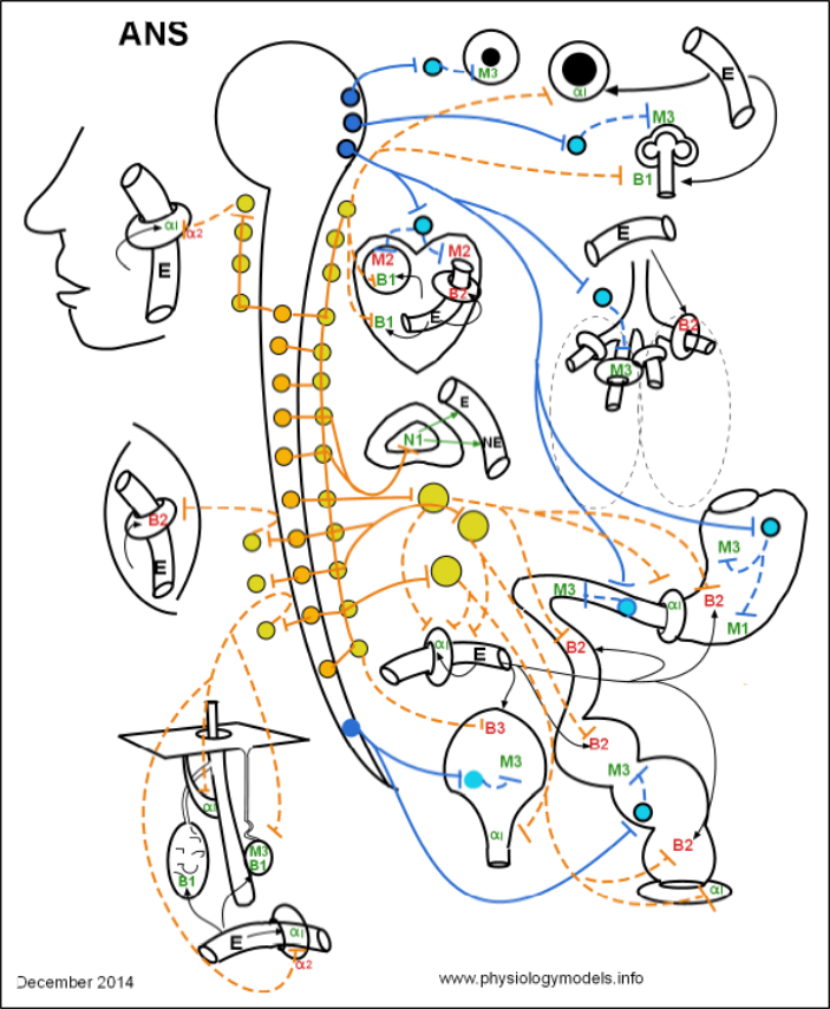
Ganglia
Ganglia are groups of postganglionic (light-blue) cell bodies. This is where the preganglionic axons secrete acetylcholine onto these cell bodies. The acetylcholine binds to and activates receptors on the cell bodies. As a result, the postganglionic neurons send impulses down their axons causing their terminals to also release acetylcholine onto the cells comprising the organ.
Because the axons of PSNS preganglionic neurons (solid lines) are long, the location of postganglionic cell bodies are near or within the target organs. In these ganglia they synapses with postganglionic cell bodies (light-blue circles) that have short axons (dashed lines) spreading throughout the organ.
When the ganglia are within a target organ they are referred to as intramural ganglia as shown in the stomach. Intramural means 'within the wall'. When the ganglia are on or near the outer surface of a target organ they are referred to as terminal as shown near the heart.
Organs
For this tutorial the term 'visceral' means all organs except those in the dermis and skeletal muscles; we'll consider those to be 'somatic'. It is not the organ itself but rather specific cell types within the organ that are innervated. These cell types are:
Sympathetic Division / Thoracolumbar Outflow
Nerve Anatomy
The cell bodies of the first or preganglionic neurons (orange circles) are located within the thoracolumbar region of the spinal cord in the lateral grey horns. Their axons ( orange lines) leave the cord to synapse within ganglia with the cell bodies of the second or postganglionic neurons (yellow circles); axons of these neurons are shown as dashed orange lines.
Organs
The term 'visceral' means internal organs and excludes the small organs located in the dermis ... those are referred to as 'somatic'. Keep in mind that it is not the organ itself, but rather specific cells within the organ, that are innervated. These cell types are:
Ganglia
As in the parasympathetic division the cell bodies of the postganglionic neurons are clustered together to form ganglia. Similarly it is acetylcholine that is secreted onto these cell bodies by the terminals of the preganglionic neurons. The response of the postganglionic neurons is to secrete norepinephrine onto the individual cells that comprise the organ.
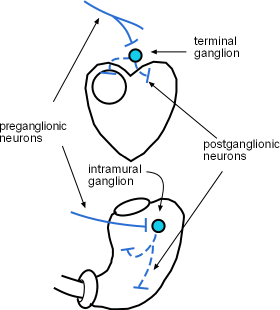
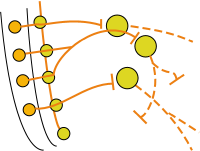
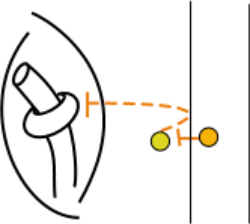
Paravertebral or Chain Ganglia
Innervation of Visceral Organs
Two chains of ganglia lie along each side, i.e. paravertebral, of the spinal cord --only one is shown in the entire model ... except in the cervical (neck) region. Each ganglion is a cluster of postganglionic cell bodies ( yellow circles). The nerve that links the ganglia into a chain consists of hundreds of preganglionic axons (orange lines) running up and down between the ganglia. The entire structure is called the ganglionic chain.
A detail of this situation is shown here where a preganglionic axon (solid orange line) exits the spinal cord. In this illustration it does not synapse in the nearest ganglion (yellow circle) but instead turns upward and passes through several other ganglia before finally synapsing in the top one. A postganglionic axon (dashed orange line) exits this ganglion to innervate smooth muscle cells encircling a blood vessel. We know that this blood vessel is within the body cavity (visceral) because the postganglionic axon goes directly from the ganglion to the target. The significance of this observation will become clear in the next section.
Innervation of Somatic Organs
In this tutorial we will use the term 'somatic' to refer to any region of the body that is not actually within the body cavity ... organs within that cavity are 'visceral'. The three illustrations at the left side of the entire model ... face, a skeletal muscle, skin structures ... represent somatic structures of the body.
This insert from the model shows the pre- and postganglionic neurons leading to smooth muscle encircling a blood vessel within a skeletal muscle. Notice how the postganglionic axon (dashed orange line) appears to turn back toward the spinal cord before heading to its target in the somatic region of the body. Details of this arrangement are described in "Somatic Targets."
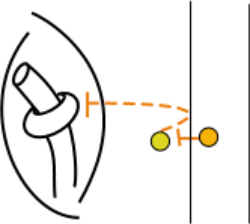
Innervation of the Adrenal Medulla
The exception to the 'two neuron rule' is the innervation of the adrenal medulla shown in this insert There are no postganglionic neurons involved...there are only preganglionic neurons (orange). Their axons exit the cord, pass through the nearest sympathetic ganglion (yellow circle) of the chain, penetrate the cortex (i.e., outer most part) of the gland to terminate within the medulla (i.e., inner most part) of the gland.
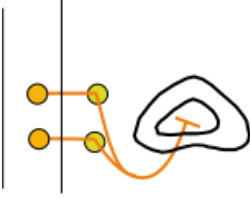
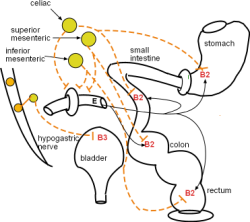
Prevertebral or Collateral Ganglia
The next insert shows three large, yellow circles; these represent prevertebral/collateral ganglia which are at the midline of the body near the aorta. They are called "prevertebral" because they lie "in front of the vertebrae." They are also called "collateral" which means "running side by side" because preganglionic neurons from both the right and left side of the spinal cord come together in these midline ganglia. The top ganglion is called the celiac, the middle is called the superior mesenteric, and the lower is called the inferior mesenteric. Their names are derived from the arteries they are near.
The insert to the left depicts the basic pattern that the two-neuron pathway uses to reach targets in the abdominal and pelvic regions. Preganglionic axons (orange line) pass through nearby paravertebral/chain ganglia (small yellow circles) after exiting the spinal cord. The nerves containing these axons are referred to as 'splanchnic' meaning 'related to visceral organs; usually those below the diaphragm'. From top to bottom they are named the greater, lesser and least splanchnic nerves.
These preganglionic axons are longer than typical ones and they continue toward the midline of the body where collateral ganglia (large yellow circles) are located. Postganglionic axons (dashed orange lines) exit the ganglia and proceed to organs of the gastrointestinal tract and urinary bladder.
The normal activity of a cell can be increased or decreased by a neurotransmitter ('from a neuron') or hormone ('from the blood'). This is due to the specific receptors on the cell membrane. In the model, some receptors are green ... indicating their normal activity will increase when stimulated ... while other receptors are red ... indicating they will decrease their normal activity . In this tutorial we will refer to the green receptors as 'stimulatory' and the red receptors as inhibitory.
It is common to refer to these relationships as either direct or inverse. It is direct relationship means an increase in the neurotransmitter/hormone will cause an increase in target cell activity ... due to 'stimulatory' receptors on the cell membrane. A relationship is inverse if an increase in the neurotransmitter/hormone will cause a decrease in target cell activity ... due to inhibitory receptors on the cell membrane.
Cholinergic Receptors
Cholinergic means "having to do with acetylcholine". The neurotransmitter acetylcholine is released from the terminals of both pre- and postganglionic neurons of the PSNS but from only the preganglionic neurons of the SNS. There are two categories of cholinergic receptors that respond to the presence of acetylcholine-- nicotinic and muscarinic.
Nicotinic Receptors
Nicotine injected into laboratory animals causes some organs to respond as if acetylcholine had been injected. Thus, the receptors to which both acetylcholine and nicotine can attach are called "nicotinic." There are several subtypes of nicotinic receptors but only the N1 variety is associated with the autonomic nervous system.
Nicotinic 1 Receptors
N1 receptors are located on all postganglionic cell bodies and on cells of the adrenal medulla.
Further down is a typical long parasympathetic preganglionic (dark blue) axon. It synapses with parasympathetic postganglionic cell bodies within an intramural (buried within tissue) ganglion. These responds by releasing their own transmitters.
Muscarinic Receptors
Muscarine, derived from the mushroom Amanita muscaria, injected into laboratory animals causes some organs to respond as if acetylcholine had been injected. Thus, the receptors to which both acetylcholine and muscarine can attach are called "muscarinic."
Of the five known subtypes, M4 and M5 are restricted to the brain. The subtypes associated with the ANS are M1, M2 and M3. Binding of acetylcholine to M1 and M3 receptors causes an increase the activity of the cell. Binding of acetylcholine to M2 receptors causes a decrease the activity of the cell. The main model shows M1 receptors only on gastric glands lining the stomach, M2 receptors only in the heart and M3 receptors located at numerous sites.
M1 Receptors
Acetylcholine activates M1 receptors on gastric glands increasing the secretion of acidic 'gastric juice' into the lumen of the stomach. The relationship between acetylcholine and the gland is direct.
M2 Receptors
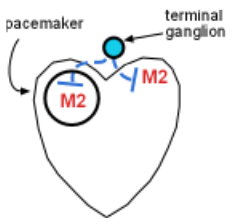
The relationship between acetylcholine and the response of these targets is inverse; binding of acetylcholine to M2 receptors causes both the heart rate and the contractile force to decrease.
M3 Receptors
Inspect the model to view M3 receptors found in many locations. Acetylcholine activation of M3 receptors results in increased responses in these organs. Responses are:
- constriction of the pupil
- increased salivation
- increased air flow
- increased gastrointestinal activity
- urinary bladder contraction
- stimulation of eccrine sweat glands.
Adrenergic Receptors
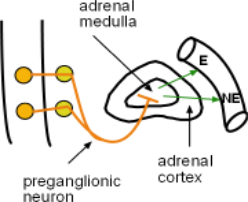
Adrenaline is secreted by the adrenal medulla.Adrenaline was the original name for what we now call epinephrine. Stimulation of the adrenal medulla by the sympathetic nervous system causes the secretion of both epinephrine (E) (80%) and norepinephrine (NE)(20%) into the bloodstream.
There are two categories of adrenergic receptors: alpha and beta. There are also subtypes of each. Useful generalizations concerning these are:
- Activation of alpha 1 and beta 1 receptors cause stimulatory responses
- Activation of alpha 2 , beta 2 & beta 3 receptors cause inhibitory responses
- NE causes a greater response than E (NE>E) when activating alpha 1 receptors
- E causes a greater or equal response than NE (E>=NE) when activating alpha 2 receptors
- E and NE cause equal responses (E=NE) when activating beta 1 receptors
- E causes a significantly greater response than NE (E>>NE) when activating beta 2 receptors
Alpha Receptors
Alpha 1 Receptors
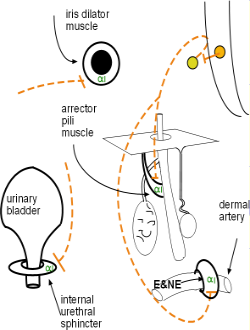
Alpha 1 receptors are more responsive to NE than to E. This is interesting as alpha 1 receptors are abundantly found on vascular smooth muscle (donuts around blood vessels) as seen in the model. The relationship between the activated receptor and the cell's response is direct -- the activity (contraction of circular smooth muscle) is increased thus reducing blood flow. Alpha 1 receptors are located on:
- all vascular smooth muscle, although densities vary throughout the body
- GI & urinary sphincters
- dilator muscle of the iris
- arrector pili muscle of hair follicles
Increase in tone of vascular smooth muscles reduces the ability of blood pressure to expand vessel diameter thus reducing blood flow to downstream organs. Increased tone in urinary and gastrointestinal sphincters reduces the passage of contents past them. Increased tone of the dilator muscle of the iris enlarges the pupil. Increased tone of arrector pili muscles pulls on the hair follicle causing hair to 'stand on end'.
Alpha 2 Receptors
Alpha 2 receptors (not shown in the model) are located adjacent to secretory terminals of some neurons mostly within the CNS. Current research is involved with determining if alpha 2 receptors are located elsewhere.
Beta Receptors
Beta 1 Receptors
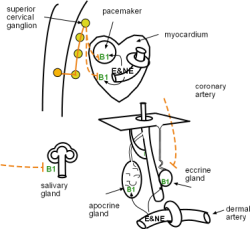
The relationship between beta 1 activation by E and/or NE is direct -- the cell's activity is increased. Beta 1 receptors are located on:
The cardiac pacemaker responds by increasing the heart rate. Simultaneously the myocardium contracts more forcefully. The physiology of the response of salivary duct cells to beta 1 activation is unclear; it appears that beta 1 activation of certain duct cells reabsorbs some water in the slowly passing saliva making it more viscous. The secretory portion of both types of sweat gland is stimulated only by E and NE from the blood, not via nerves.
Note that beta 1 activation in the heart is both neural and hormonal. In the salivary glands the activation is solely neural while in both type sweat glands it is solely due to E and NE in the blood.
Beta 2 Receptors
Beta 2 receptors are located on smooth muscle. The relationship between E (hormonal) / NE (neurological) activation and the response of the cell is inverse -- activity (muscle tone) of the cell is decreased. Beta 2 receptors are located on smooth muscle in:
- the gastrointestinal tract
- the urinary bladder
- skeletal muscle arteries
- the bronchial tree
- some coronary vessels
The model shows the main locations of beta 2 receptors throughout the GI tract -- stomach, small intestine, colon, rectum. Their activation results in decreased muscle tone and motility. In the urinary bladder this decreased muscle tone enables greater filling.
The model shows relaxation of the circular smooth muscle in the bronchial tree is due to epinephrine -- note the lack of innervation at this location thus NE is not indicated. Beta 2 receptors are also on small coronary arterioles thus increasing hormonally induced blood flow within the musculature of the heart. These receptors are the primary receptor in skeletal muscles arteries resulting in enhanced blood flow especially when epinephrine is present.
The model shows which arteries have alpha 1 sites and which have beta 2 sites. Remember that epinephrine is the best activator of B2 sites.
Beta 3 Receptors
The 'rare' beta 3 (B3) receptors on the smooth muscle cells of the urinary bladder decrease muscle tone in response to receptor activation thus enabling increased filling.
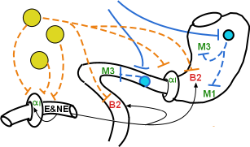
ANS Targets in the Head
The model illustrates several organs in the head: arteries of the oral and nasal mucosae, the iris of the eyes and salivary glands.
Arteries of the Nasal & Oral Mucosae
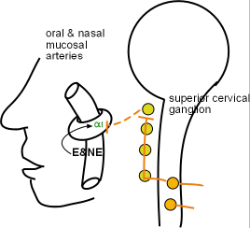
These arteries supply the lining (mucosa) of the mouth and nasal cavities. Arterial diameter is due to blood pressure pushing against the arterial wall. If the tone of the encircling smooth muscle is increased the diameter can't expand as much thus restricting downstream blood flow. If this tone is decreased then blood pressure can expand the diameter and increase blood flow.
Sympathetic nerves arising from the superior cervical ganglion innervate the encircling smooth muscle of these arteries. Norepinephrine activated alpha 1 receptors cause the cells to increase their tone and decrease blood flow. Epinephrine, from the adrenal medulla, is especially potent in further increasing this tone resulting in additional vasoconstriction. The result is 'dry mouth' and 'ease of nasal air flow' that is part of the 'fight-or-flight' response characteristic of a high level of sympathetic activity. Notice there is no parasympathetic innervation at this site.
Iris of the Eye
Click on 'Model' for larger view.
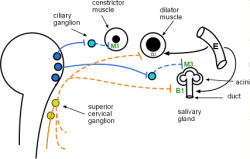
The iris contains two intertwined layers of smooth muscle cells. The constrictor cells are arranged in a donut pattern ... like in the vasoconstrictor muscle cells of arteries. Thus, when stimulated to contract, the encircled pupil will become smaller causing miosis. This behavior is due to PSNS activity secreting acetylcholine on the M3 receptors of these muscle cells.
The dilator cells are arranged like spokes on a wheel and radiate outward away from the pupil. Thus, when stimulated, they cause the pupil to dilate (mydriasis). This behavior is due to alpha 1 receptors that are activated by secretion of NE from SNS nerves arising from the superior cervical ganglion of the sympathetic chain. Additionally, they can be stimulated by E released into the bloodstream from the adrenal medulla.
Salivary Glands
The above insert also depicts a functional unit of a salivary gland. Salivary glands have flask-shaped acini of glandular cells with M3 receptors and 'duct cells' with B1 receptors. The 'acini cells' secrete amylase and/or mucus, along with fluid the consistency of blood plasma, into their hollow centers. The 'duct cells' modify the composition of the passing saliva. Both divisions of the ANS are involved in the behavior of these glands ... the acini are activated by the PSNS while the duct cells are activated by the SNS.
Saliva is constantly produced because both divisions are always working simultaneously. The volume and consistency of the saliva depends on which division predominates at the given moment.
Acetylcholine activation of muscarinic 3 receptors on the glandular acini increases the secretion of saliva resulting in a high volume of watery saliva. This is characteristic of the 'rest-and-digest' response when parasympathetic activity dominates.
Neural norepinephrine activation of B1 receptors in certain duct cells results in low volume, viscous saliva. There is a good blood supply to these glands so that blood-borne epinephrine decreases the volume even further under excessive sympathetic stimulation. The resulting 'dry mouth' is characteristic of the 'fight-or-flight' response at such times.
Targets in the Thorax
The myocardium, consisting of cardiac muscle, is the contractile part of the heart; the pacemaker (circle inside heart) consists of autorhythmic cells that establishes the heart rate. The coronary arterioles shown within the heart muscle are not the large coronary arteries that lie on the surface of the heart. These smaller arterioles are embedded within the myocardium. This organ is neutrally regulated by both divisions of the ANS as well as hormonally.
Heart
Parasympathetic Innervation
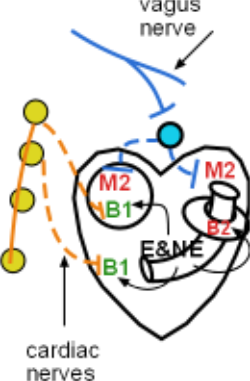
Pacemaker
The pacemaker can function without any innervation because it has an intrinsic mechanism that establishes a baseline heart rate. However, acetylcholine released from parasympathetic postganglionic neurons (dashed blue line) binds to muscarinic 2 receptors decreasing this rate. These axons arise from a terminal ganglion (light blue circle) near the surface of the heart. The preganglionic neurons (solid blue line) from the brain travel to this site within the vagus nerve.
Myocardium
The heart's atria (upper chambers) also have muscarinic 2 receptors. When acetylcholine binds to these cells their force of contraction is decreased. There appears to be little parasympathetic innervation of the heart's ventricles (lower chambers).
Sympathetic Innervation
Pacemaker
Chronotropism refers to a change in rate ... in this case, heart rate. Norepinephrine released from postganglionic neurons (dashed orange lines) binds to beta 1 receptors in the pacemaker resulting in an increased heart rate. These neurons arise from several ganglia (yellow circles) in the cervical region of the ganglionic chain. The preganglionic neurons (solid orange line), originating in the thoracic spinal cord, travel upward through the chain to reach these cervical ganglia.
Myocardium
Inotropism refers to a change in force ... in this case, the force of contraction. Cardiac muscle cells of both the atria and ventricles have beta 1 receptors. Norepinephrine released from postganglionic neurons (dashed orange lines) binds to these receptors resulting in increased contractile force. Here, too, the preganglionic neurons arise from the thoracic cord and travel upward through the chain to the cervical ganglia.
Hormonal Control
In fight-or-flight situations both norepinephrine and epinephrine will diffuse from cardiac capillaries to bind with beta 1 and beta 2 receptors. Positive chronotropic and inotropic responses increase both heart rate and contractility. There are beta 2 receptors on the smooth muscle encircling coronary arterioles resulting in decreased muscle tone of the vascular wall increasing cardiac blood flow. This facilitates bringing E and NE to the heart; recall that epinephrine's effect on the heart is significantly more potent than norepinephrine alone.
Respiratory System
The parasympathetic division (blue neurons) is the dominant neural control mechanism of this system -- there is no direct sympathetic neural involvement. Local controls play the major role in the regulation of this system. (Refer to Respiratory System in the main menu of this site).
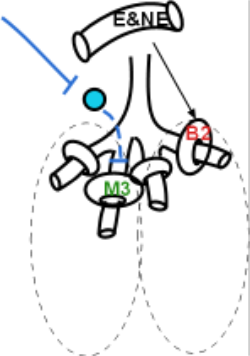
Parasympathetic Innervation
Neural Control
The PSNS preganglionic neurons that reach the respiratory tree travel within the vagus nerve. They synapse with terminal ganglia (light blue circle) within the lungs. The postganglionic neurons from these ganglia (dashed blue line) release acetylcholine on M3 receptors on smooth muscle encircling the smaller cartilage-free bronchioles. PSNS activation causes an increase in the tone of these muscles causing bronchoconstriction and breathing difficulty. There is no SNS innervation of these smooth muscles!
Hormonal Control
However, mixed in with the M3 receptors are also beta 2 receptors on these smooth muscle cells. They are activated when epinephrine and norepinephrine diffuse to them from the bloodstream ... part of the fight-or-flight mechanism. As before, recall that beta 2 receptors are significantly more responsive to epinephrine than norepinephrine. When the muscle tone of these smooth muscle cells decreases it is easier for these airways to expand when during inhalation.
Targets in the Abdomen
Splanchnic Nerves & Collateral Ganglia
"Splanchnic" means having to do with the viscera (i.e., internal organs). Sympathetic preganglionic axons (solid orange lines) emerge from the cord and pass through ganglia of the sympathetic chain (line of yellow circles) without synapsing. They gather into three nerves called the greater, lesser & least splanchnic nerves. Though not obvious in the model the greater consists of bilateral outflow from T5-9, the lesser of outflow from T 10 & 11 and the least from T 12.
Parasympathetic preganglionic axons (solid blue line) emerge from the sacral region of the cord to form the pelvic splanchnic nerve. These neurons penetrate pelvic organs to synapse with intramural ganglia (light blue circle). From here, postganglionic axons (dashed blue line) synapse with their receptors within the organ.
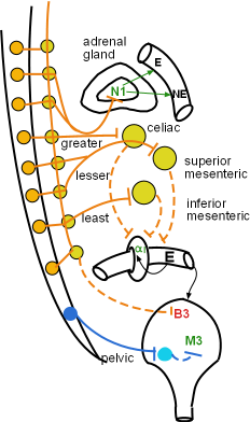
The three large ganglia (yellow circles) are named the celiac, superior mesenteric and inferior mesenteric. They sit just ventral to the aorta and the nerves entering and leaving them are intertwined forming a plexus. This entire region is called the 'solar plexus'. Within these ganglia preganglionic neurons release acetylcholine on nicotinic 1 receptors (not shown) on cell bodies of postganglionic neurons. These neurons respond by sending impulses down their axons to release norepinephrine on the organs they innervate. An example is the innervation of an abdominal vessel shown in the insert.
Adrenal Medulla
The adrenal medulla is unique because it is the only organ directly innervated by preganglionic axons (solid orange line), instead of postganglionic axons. These preganglionic axons form a branch of the greater splanchnic nerve as indicated in the model. Acetylcholine activation of nicotinic 1 receptors of chromaffin cells in the medulla increases their secretion of epinephrine (80%) and norepinephrine (20%) into capillaries as indicated by the green arrows. It is this release that is a hallmark of the "fight-or-flight response".
Gastrointestinal Tract
This organ system contains a nervous system of its own called the enteric (i.e., intestinal) nervous system; some classify this as a third division of the autonomic nervous system.
Stomach
Click on 'Model' for larger image.
Parasympathetic Innervation
Smooth Muscle
The vagus nerve contains parasympathetic preganglionic neurons (solid blue lines) that penetrate the stomach wall to synapse within a plexus of postganglionic cell bodies (light blue circle). This plexus (myenteric/Auerbach's) lies between the outer longitudinal and inner circular smooth muscle layers (not shown) of the stomach wall. When stimulated by acetylcholine from the preganglionic neurons, the postganglionic neurons will secrete acetylcholine that activates muscarinic 3 receptors on smooth muscle of both muscle layers. The result is increased motility of the stomach.
Gastric Glands
Another plexus lies between the circular smooth muscle layer and the mucosa. The axons of these parasympathetic postganglionic neurons connect with mucosal gastric glands that bear muscarinic 1 receptors. Acetylcholine-activated M1 receptors cause an increase in gastric juice secretion.
Sympathetic Innervation
Smooth Muscle
The celiac ganglion (top yellow circle) houses the cell bodies of sympathetic postganglionic neurons whose axons (dashed orange lines) lead to beta 2 receptors of both muscle layers of the stomach wall. Norepinephrine-activated beta 2 receptors cause decreased motility of the stomach wall. Other neurons innervate the pyloric sphincter releasing norepinephrine onto the alpha 1 receptors located on these smooth muscle cells. When activated by NE they respond by increasing their tone making passage of material from the stomach to the intestine more difficult.
Gastric Glands
Note that there are no sympathetic postganglionic neurons innervating the gastric glands (location of M1 receptors).
Intestines
Parasympathetic Innervation
Like the stomach, the duodenum (proximal small intestine) is innervated by branches of the vagus nerve (solid blue line). Synapses occur within the myenteric plexus (light blue circle). Acetylcholine released from postganglionic neurons (dashed blue lines) ... also called enteric neurons ... binds with muscarinic 3 receptors on the intestinal smooth muscle to increase motility.
The remainder of the small intestine has little parasympathetic innervation. However, the colon and rectum do have parasympathetic innervation from the pelvic nerve (solid blue line). Again, the postganglionic neurons are the enteric neurons of the myenteric plexus. The smooth muscle receptors are muscarinic 3 and activation by acetylcholine increases motility in these sections.
Click on 'Model' for larger image.
Sympathetic Innervation
The jejunum and ileum are innervated by postganglionic axons (dashed orange line) originating in the celiac ganglion. The colon (large intestine) is innervated by neurons from the superior mesenteric ganglion while in the rectum they originate in the inferior mesenteric ganglion. Norepinephrine is released from these to binds with beta 2 receptors on the smooth muscle layers to decrease their motility. Additionally, neurons from the inferior mesenteric also innervate the internal anal and urethral sphincters releasing norepinephrine on alpha 1 receptors causing increased tone in those tissues.
Splanchnic Arteries
The sympathetic division controls arterial blood flow in the abdominal cavity. The circular smooth muscle encircling the arteries supplying the gastrointestinal tract have alpha 1 receptors. They are innervated by sympathetic postganglionic neurons (dashed orange lines). There are many splanchnic arteries with innervations originating in all three collateral ganglia (i.e., solar plexus). Norepinephrine-activated alpha 1 receptors cause the encircling smooth muscle to constrict reducing blood flow to the GI tract. Blood-borne epinephrine (E) has the same effect. There is no parasympathetic innervation.
Urinary Bladder
Parasympathetic Innervation
The preganglionic neurons (solid blue line) of the pelvic splanchnic nerves innervate the bladder wall. They secrete acetylcholine onto the cell bodies of postganglionic neurons within intramural ganglia (light blue circle) in the wall. Postganglionic axons (dashed blue line) release acetylcholine to activate muscarinic 3 receptors on smooth muscle cells. These cells respond by increasing their tone so that the bladder is not as compliant to filling.
Sympathetic Innervation
The bladder wall musculature also has beta 3 receptors that are innervated by postganglionic neurons from the hypogastric nerve arising from the ganglionic chain. Activated beta 3 receptors cause decreased muscle tone in the bladder that facilitates filling.
The smooth muscle of the neck of the bladder (internal urethral sphincter) has alpha 1 receptors. Activation by norepinephrine from postganglionic neurons arising from the inferior mesenteric ganglion causes an increase in tone helping to retain the urine in the expanding bladder.
Targets in the Somatic Region
'Somatic' means the body wall as opposed to the internal viscera. Inspection of the model indicates that these organs are structures in the dermis (arrector pili muscle of hair follicles, eccrine sweat glands and dermal arteries) ,arteries in skeletal muscles, and oral and nasal mucosae.
The insert shows a very short preganglionic axon (solid orange line) leaving the spinal cord to synapse with a postganglionic cell body (yellow) in the ganglionic chain. The postganglionic axon (dashed orange line) appears to curve back to contact the spinal cord before heading to its target is in the somatic region of the body.
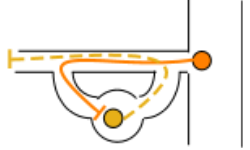
This insert, not shown in the model, has lines drawn around the neurons to show the nerve in which they are housed. There are two short connections to the main nerve are called rami ... branches. The branch containing the preganglionic axon (solid orange line) is called the white ramus ... white because the axon is myelinated. Myelination is due to a lipid-rich (thus the white color) Schwann cell wrapping around the axon to form a cinnamon-roll like covering. The branch containing the postganglionic axon (dashed orange line) is called the grey ramus ... because its axon is not myelinated and neurons are grey in color. It re-enters the main nerve to travel to the somatic region of the body.
Click on 'Model' at the left and note the lack of parasympathetic neurons in this region.
Blood Vessels
The vast majority of somatic vessels are within skeletal muscles shown center left in the model. The encircling smooth muscle has beta 2 receptors. Neural activation of beta 2 receptors by norepinephrine causes a decrease in tone of these muscles and vasodilation results in increased blood flow. Under high sympathetic activity (fight-or-flight response) epinephrine diffusing from the blood enhances this response -- remember that B2 receptors respond more strongly to epinephrine than to norepinephrine.
Dermal Structures
Arrector Pili Muscle
These small smooth muscles originate on the lower surface of the epidermis and insert on the side of dermal hair follicles. Follicles are not part of the actual hair but are tubular depressions that house much of the hair. Norepinephrine-activated alpha 1 receptors increases the tone of these cells. The response is that the follicle is pulled such that the enclosed hair sticks up straighter (hair standing on end) and some of the skin is pushed up into a bump (Goose bump).
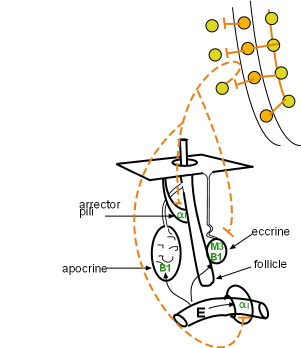
Sweat Glands
Eccrine
The most abundant and widespread type of sweat gland is the eccrine gland. Their ducts lead directly to a pore at the surface of the skin. Neural activation of muscarinic 3 receptors on the secretory cells of these glands causes increased production of a watery secretion primarily useful in thermoregulation -- evaporation of sweat from the skin surface decrease body heat. The postganglionic neurons (dashed orange lines) innervating these glands is 'an exception to the rule' because they secrete acetylcholine instead of the expected norepinephrine. Because of this they are classified as cholinergic sympathetic nerves.
The secretory cells of eccrine sweat glands also have beta 1 receptors. However, there is no sympathetic adrenergic (i.e., norepinephrine) innervation. Epinephrine from the bloodstream, released during the 'fight-or-flight response', is responsible for the production of 'nervous' sweat' from these glands. Notice that simultaneously epinephrine is causing vasoconstriction of the dermal blood vessels resulting in the 'white with fright' appearance so characteristic of this state.
Apocrine
Apocrine sweat glands are predominantly located in the armpits and groin area. Their ducts do not lead to pores at the surface but rather into the side of hair follicles. From there the sweat is moved to the surface. The secretion is thick and contains many organic compounds that bacterial break down producing a foul odor. There is no innervation to these glands. Epinephrine stimulated beta 1 receptors induce production of this type sweat.