Respiratory Tutorial
Ventilation & Perfusion
The purpose of pulmonary ventilation is to take in oxygen, to distribute it to the tissues, and pick up and eliminate carbon dioxide waste. According, this tutorial will begin with a description of how red blood cells carry these respiratory gases between the tissues and the lungs.
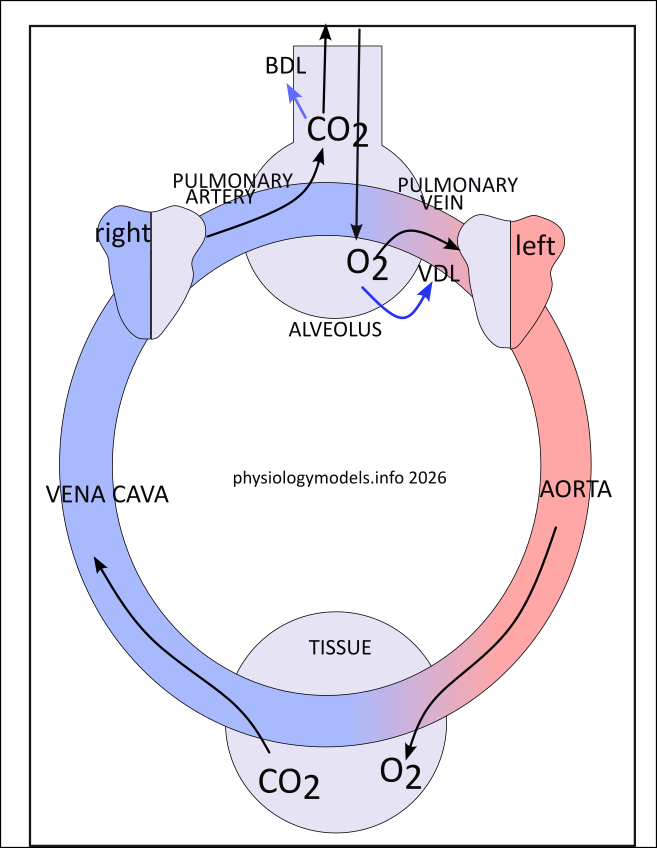
The illustration shows a 'flask' at the top representing an alveolus (air sac) and the circle at the bottom is a tissue cell. The large colored circle is the circulatory system; blue blood has a high carbon dioxide concentration and red blood has a high oxygen concentration.
The heart is actually two separate pumps. The right half pumps deoxygenated (blue) blood to the lungs while the right half pumps oxygenated (red) blood to the rest of the body. Vessels carrying blood toward an organ are called veins while vessels leaving it are called arteries.
Pulmonary Circuit
The pulmonary circuit perfuses the lungs with blood where carbon dioxide is released and oxygen is taken in; its pump is the right half of the heart. Oxygen changes the color of hemoglobin in the red blood cells from dark red (blue) to bright red, as shown in the illustration. As carbon dioxide (CO2) is expired through the airways it causes them to dilate (bronchodilation (BDL)). Inspired oxygen (O2) causes vessels leading to the left half of the heart to dilate (vasodilation (VDL)).
Systemic Circuit
The systemic circuit perfuses all the other organs. Its pump is the left half of the heart. As blood passes through tissues, metabolism extracts the oxygen and adds carbon dioxide changing the color of hemoglobin. The illustration labels the veins and arteries of each circuit; 'output' vessels are veins while 'imput' vessels are arteries. Notice the difference on hemoglobin color in veins and arteries in the two circuits.
In the Tissues...the Bohr Effect
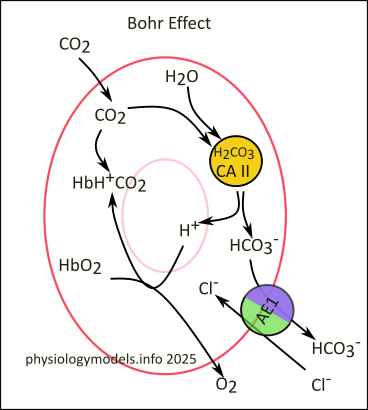
The job of hemoglobin is to transport oxygen from the lungs to the tissues and transport carbon dioxide from the tissues to the lungs. The reactions that occur within the red blood cell (RBC) are identical, but reversed, in the two trips.
Within the RBC, the enzyme carbonic anhydrase (CAII) rapidly combines incoming carbon dioxide with water forming carbonic acid (H2CO3). This acid is very unstable and immediately ionizes to hydrogen and bicarbonate (H+ + HCO3-). The bicarbonate is transported out of the RBC, by AE1 transporters, in exchange for chloride from the plasma (chloride shift.)
The hydrogen is buffered by oxyhemoglobin (HbO2 and the oxygen is released when this occurs. In its buffered condition, hemoglobin binds dissolved carbon dioxide becoming carbaminohemoglobin (HbH+CO2).
While in the RBC, 70%-90% of the carbon dioxide that enters the RBC will be converted to bicarbonate (HCO3-) and the remaining 10%-20% will be split between carbaminohemoglobin (HbH+CO2) and that remaining dissolved in the cytoplasm.
***************************
In the Lungs...the Haldane Effect
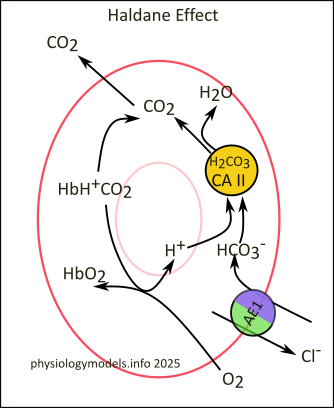
Entering the capillaries in the lungs, the massive influx of oxygen binds to carbaminohemoglobin (HbH+CO2) causing the release of both hydrogen and carbon dioxide; oxyhemoglobin (HbO2) is formed in its place. However, this releases only a small percentage of the carbon dioxide picked up in the tissues.
Most of the carbon dioxide is transported as bicarbonate and will be converted back into carbon dioxide to be exhaled. This is accomplished by AE1 causing a reverse chloride shift that uploads bicarbonate into the RBC. There, it encounters CAII that combines it with hydrogen. When these two reactants are bound to CAII they are converted to carbonic acid that ionizes to carbon dioxide and water. The carbon dioxide diffuses into the plasma to be exhaled at the lungs.
***************************
Lung Anatomy
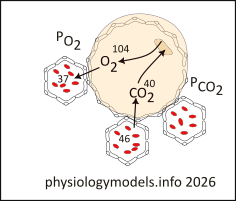
The pulmonary airways end in thin-walled sacs called alveoli; there are ~300 million in each lung. A section through a lung would resemble a sponge. Covering each alveolus is a network of thin-walled capillaries shown here in cross-section. Oxygen and carbon dioxide diffuse, along their partial pressure (P mmHg) gradients, through the double-layer of cells between an alveolus and a capillary. Leaving the lungs, blood gas partial pressures are O2= 75-100mmHg and CO2 = 35-45mmHg.
The inflation of the alveoli is due to the inflation of the lung. Imagine you put super glue on your hands then hold an inflated balloon (don't try this). As you try to enlarge the balloon it becomes harder and harder. The reason is that increasing the balloon's volume reduces its internal pressure (Boyle's Law) creating a negative pressure. If you opened this balloon the air would rush in along this pressure gradient. And that's how inspiration occurs, but the 'super glue' that pulls the alveoli (balloon) open is surface tension.
You can see the effect of surface tension by the rounded shape of a water drop. The water molecules are mini-magnets...one surface is slightly negative and the opposite is slightly positive. Put them together and they pull on each other; those at the surface are pulled toward the center thus the 'roundness' of the drop.
The 'sheen' of water (interstitial fluid) around the alveoli and capillaries hold them together...pull somewhere and the rest follow. Pull the surface of the lung and the volume of the alveoli increases...causing the pressure within them to fall and air to rush in. Surface tension 'pulls the surface of a lung' because it 'magnetically', via surface tension, holds the lung to the inner surface of the chest cavity.
Imagine this...take a 'magical' water mattress and fill it with a pint of water. Flatten it out and place an air-filled balloon, moistened over its surface, on top of the mattress. Gather up the edges and pull them over the balloon until all its edges meet. Now, here's the magic...the mattress edges seal together and the whole thing shrinks to snuggly fit over the balloon. Doesn't look as if there is any water in the mattress but there is. A film of water is touching the inner surface of the mattress everywhere and if you try to lift its outermost surface away the innermost surface seems stuck to it...surface tension in action. Remember moistening the outer surface of the balloon? Guess what, this moisture causes surface tension between the balloon and inner mattress surface. Pulling on the outer mattress surface will, via two layers of surface tension, expand the balloon. If there was a tube in the balloon and it was opened, air would rush in.
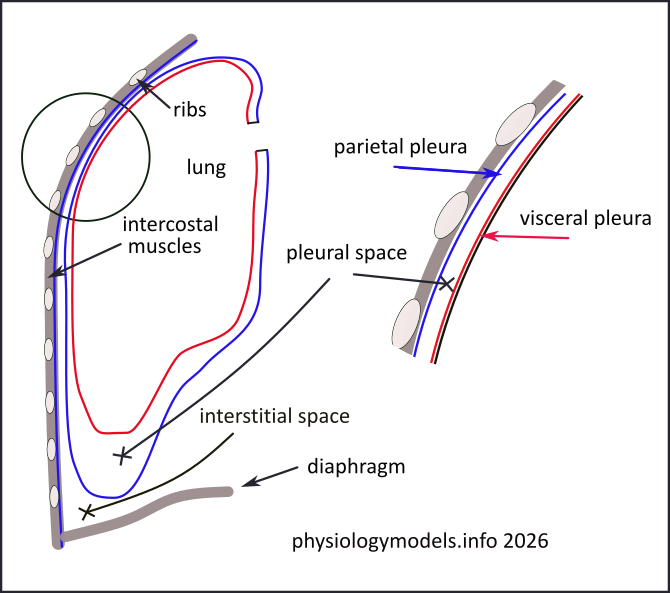
The illustration shows these surfaces. In the above analogy the balloon is the lung and the red line around it is the 'inner mattress surface'. The blue line beyond that is the 'outer mattress surface; the space between the two is the 'pint of water'. The enlargement identifies the red line as the visceral pleura and the blue line as the parietal pleura. The pleural space is filled with pleural fluid...source of the surface tension. This 'pleural-enclosed' lung fills the thoracic (chest) cavity; surrounded by interstitial ("between the tissues") fluid, surface tension holds it against the chest wall and the diaphragm. The volume of the cavity...and the lung and the alveoli...are expanded by contraction of the external intercostal muscles and the diaphragm. The drop in internal air pressure of the alveoli causes air to flow in...inspiration.
***************************
Respiratory Center
Agreement concerning neural interconnections within the brainstem respiratory centers is not universal. It is complicated and new research is ongoing. Accordingly, this tutorial will present currently-accepted neural connections that provide a useful understanding of respiratiory mechanics.
At first glance the model appears indecipherable but the this tutorial will describe the interactions as they relate to specific events. A large amount of information is 'hidden' in this model but knowing the symbolism is the key to revealing that information.
The pons and medulla, in the brainstem, contain the central pattern generator (CPG), formerly called the 'respiratory center'. It contains paired clusters of neuron cell bodies (circles) that are connected by interneurons (lines). All of these structures are paired but only one set is illustrated.
Centers and their outgoing (efferent) nerves are color-coded. The nerve starts as a dot within the center and extends as either a solid or dashed line. Targeting another center, the nerve ends in either an arrowhead or an X. The arrowhead indicates the targets 'excitability' is increased or it is activated. The X means the targets 'excitability' is decreased or it is inactivated. The excitability level indicates whether a weak or strong stimulus is required to affect the target.
Some stimuli begin gradually and build to a 'crecendo'; scientific literature refers to these as "ramps". Other stimuli start off with a 'bang' before gradually fading out. Yet others are "bursts" that are strong but stop quickly. But most are not so exciting and work quietly, and constantly, without much notice. These are the modulators that 'modify' the excitability of their targets.
How to Interpret the Symbolism
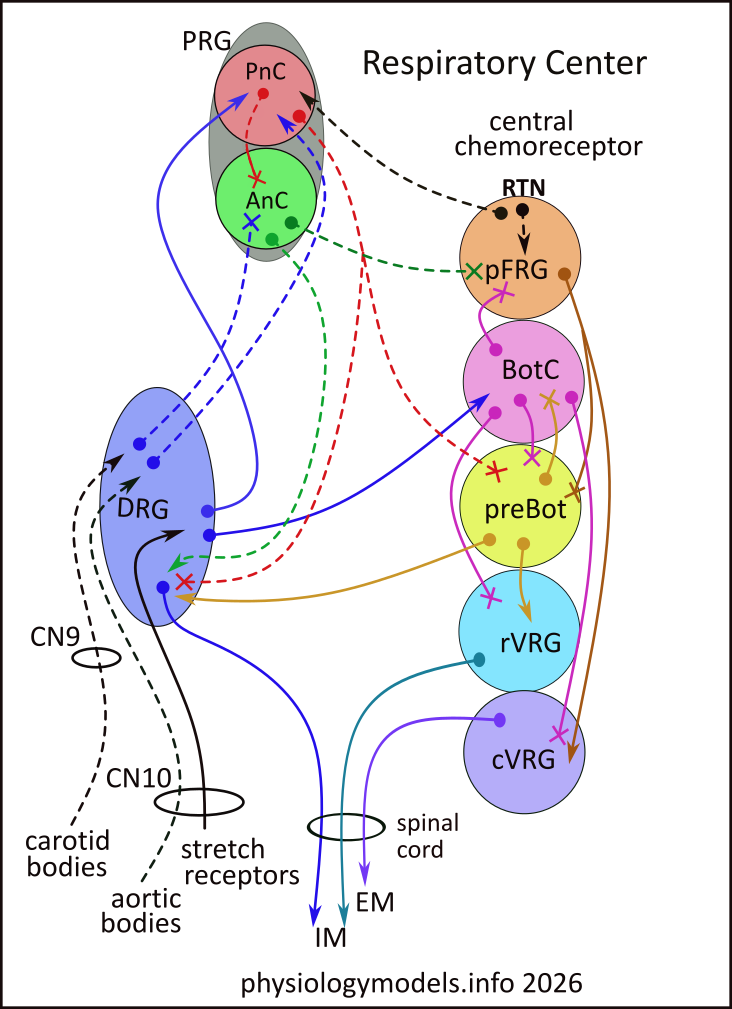
Respiratiory centers can be stimulated to (1)activate, (2) inactivate or (3) increase their 'excitabilty' level. The first two are obvious...either 'fire' the efferent (outgoing) neurons or stop firing them. The latter means to become easier to affect. The same concept applies to inhibition. The center can be inhibited to (1) stop being active, (2) stop being inactive, or (3) become harder to affect.
Solid nerves either stimulate (arrowheads) or inhibit (Xs) their targets. These signals only last for a few seconds and cause the phases of breathing...inspiration or expiration...and they are referred to as 'phasic'. The center they target will respond by either activating (firing) their efferent nerves or inactivating them if they are currently active. This assumes the centers have already been 'modulated' to respond.
Dashed nerves either make their target easier (arrowhead) or harder (X) to respond to an afferent signal. These signals are continuous (tonic). In general, when sensory input indicates that the inspiratory rate should increase, stimulating modulatory signals will become stronger and inhibitory ones weaker. Some nerves send signal tonically but can become phasic.
To illustrate how to interpret the model, the rVRG center (turquoise) has one outgoing (efferent) solid-arrowhead nerve targeting "IM" (inspiratory muscles: diaphragm and external intercostals). Whether or not this efferent nerve will 'fire', and cause inspiration, depends on the excitabilty level established by BotC.
***************************
Eupnea
Quiet, relaxed breathing (eupnea) is 12-20 breaths per minute. Air enters the lungs (inspiration) because the chest cavity expands and it leaves (expiration) when the chest passively recoils. The pairing of ventilation with perfusion (blood flow) enables the exchange of blood gases with the environment, as described above.
The brainstem centers involved in eupnea are shown the this extraction from the main model.
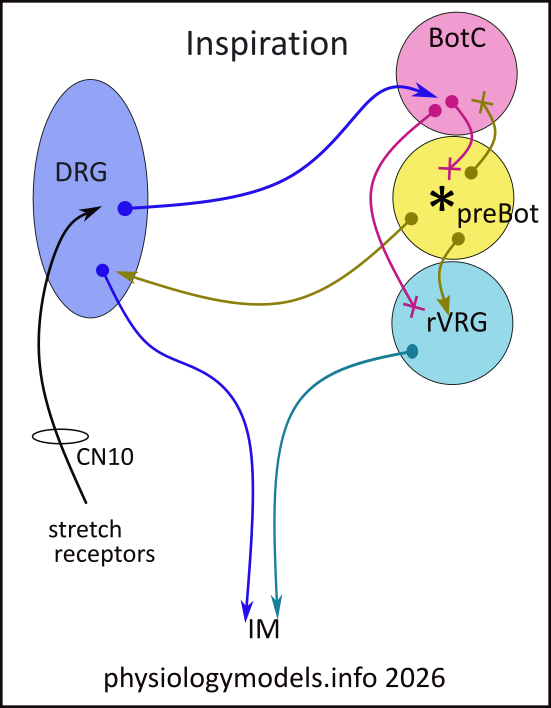 The following dialogue is derived from the symbolism in this small illustration.
The following dialogue is derived from the symbolism in this small illustration.
- Key:
- DRG = dorsal respiratory group
- BotC = Botzinger complex
- preBot = preBotzinger complex
- * = pacemaker cells
- rVRG = rostral ventral respiratory group
- IM = inspiratory muscles.
No external neural signal is required to activate preBot because it contains pacemaker cells (*). Pacemaker signals activate preBots three efferent nerves that (1) activate rVRGs efferent nerve that leads to inspiratory muscle contraction, (2) activate DRGs efferent nerve that also leads to inspiratory muscle contraction, and (3) inhibit BotC from inactivating it (preBot) and rVRG while active.
Inspiration continues for ~2 seconds while sensory receptors in the pulmonary airways track the inspiratory depth. As the chest cavity expands and airway stretch increases, afferent signals are stimulating DRG to stimulate BotC. This increased stimulation 'outcompetes' BotCs inhibition by preBot and 'fires' efferent inhibitory signals, to preBot and rVRG, that stops inspiration. This permits the chest cavity to passively recoil causing expiration. After ~3 seconds the activity of preBot pacemaker cells will initiate the next inspiration.
***************************
Inspiratory Rate & Depth
Eupnic breathing, that inspires ~500ml of air, occurs when systemic arterial blood-gas levels are within their the normal ranges...PO2 is 75-100 mmHg, PCO2 is 35-45 mmHg. If increased metabolic or physical activity occurs, the carbon dioxide levels will increase (hypercapnia) and oxygen levels will decrease (hypoxia). A return to normal values involves two changes; an increase in the rate and the depth of inspiration. The rate increase is governed by the pneumotaxic center (PnC) while the depth change is governed by the apneustic center (AnC).
Informing the respiratory centers about the blood-gas levels requires sensors. Most are found outside of the central nervous system (peripheral) and there are also 'central' receptors that sample the carbon dioxide levels in the cerebrospinal fluid (CSF).
Outside the central nervous system, the carotid bodies are found in the walls of the carotid arteries. These sensors contain the enzyme carbonic anhydrase that combines carbon dioxide and water forming carbonic acid. This acid then ionizes to bicarbonate and hydrogen ions that increases the acidity. The glossopharyngeal nerve (CN9) conveys this information to dorsal respiratory group (DRG). The aortic bodies, embedded in the arch of the aorta, activate when oxygen levels in the blood are below ~60mmHg. This information is conveyed to DRG via the vagus nerve (CN10).
The DRG functions as a sensory relay center. It combines information from peripheral chemical and stretch receptors that is sent throughout the brainstem. For example, the DRG signals the status of blood-gas levels to the grey pontine respiratory group (PRG) that contains two regions: the red pneumotaxic center (PnC) and the green apneustic center (AnC). This color-coding hints at the PnCs role as the 'inspiratory off-switch' and the AnCs roll as the 'inspiratory on-switch'.
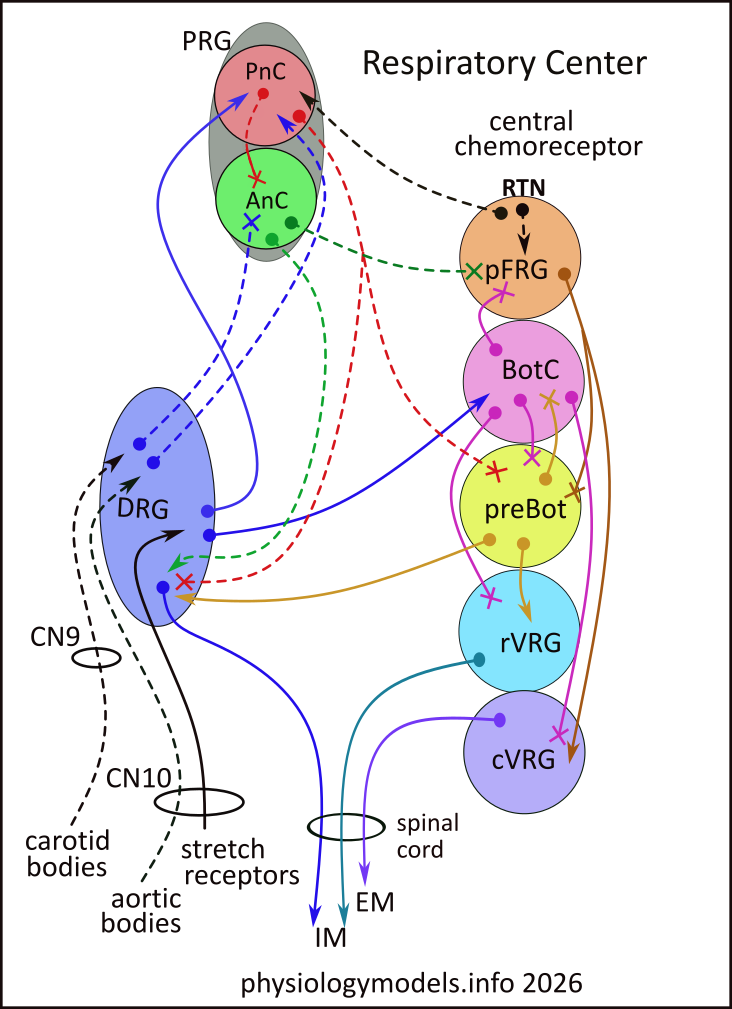
There are also central chemoreceptors at the surface of the brainstem that respond to the hydrogen ion concentration (acidity) in the cerebral spinal fluid (CSF). These are in the retrotrapezoid nucleus (RTN) that tonically transfers this information to PnC and the nearby parafacial respiratory group (pFRG); increased acidity, due to carbon dioxide, excites these targets.
PnC tonically supresses the inate excitability of AnC. The difference in excitability between these two regions is further enhances when DRG tonically stimulates PnC while inhibiting AnC. When AnC is released from inhibition it stimulates DRG to increase the depth of inspiration. This 'release' is due to PnC efferent nerves.
PnC efferents:
- inhibit AnC allowing increased inspiratory depth while supressing pFRG excitability (see below), and
- reduce the excitability of preBot and DRG to respond to stimulation that leads to inspiratory muscle contractions.
The PnC receives three sources of stimulation: (1) from DRG regarding peripheral blood-gas levels, (2) from stretch receptors, via DRG, when lung volume approaches three times normal (500ml) ...Hering-Breuer reflex, and (3) from the retrotrapezoid nucleus (RTN) in the ventral resporatory column:
- The greater hypercapnia and/or hypoxia are, the quicker PnC will stop inspiration early and cause faster inspiratory rates.
- The Hering-Breuer reflex stops inspiration and triggers expiration; it is only apparent in newborns. In adults, it's usually only noticeable during very deep breaths or exercise, not normal resting breathing.
- Increasing acidity stimulates the 'inspiratory off-switch' and stmulates pFRG to cause forced expiration.
pFRG activates forced expiration that requires contraction of abdominal and internal intercostal muscles. Nerves leading to these muscles originate in the caudal VRG (cVRG). The pFRG activates cVRG while simultaneously inhibiting preBot to prevent inspiration.
***************************
Spirograph
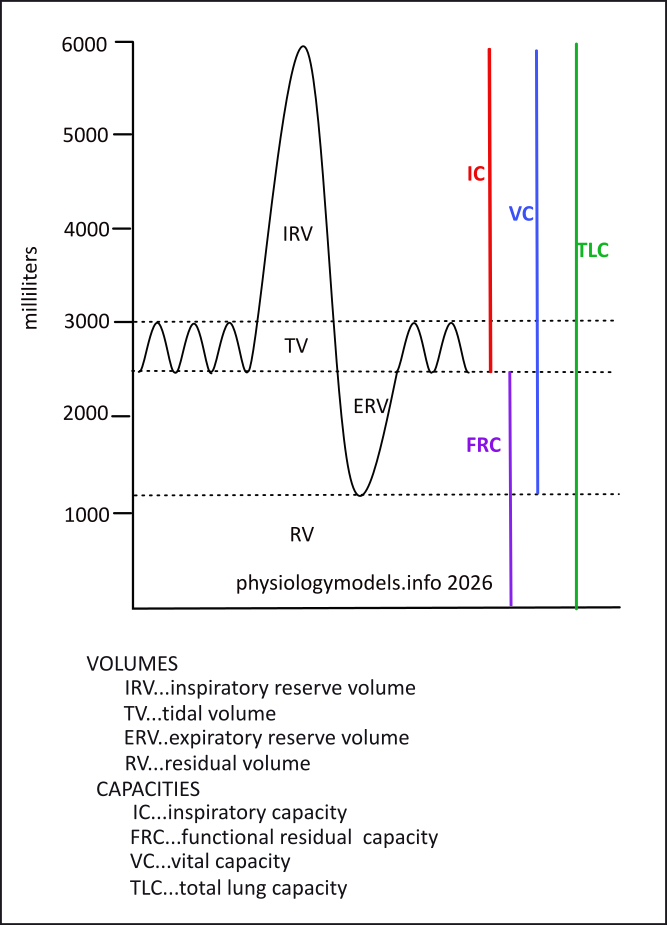
A spirograph shows the volumes of air flow during the various breathing phases. The eupnic phases of breathing, inspiration and expiration, are represented as the tidal volume (TV); the average amount is 500ml in then out. If inspiration is continued, the additional volume inhaled is the inspiratory reserve volume (IRV). The air forcefully moved following a passive expiration is the expiratory reserve volume (ERV). There is still air remaining in the lungs that cannot be expired called the residual volume (RV).
Capacities are combinations of volumes. The inspiratory capacity (IC) is a quiet inspiration plus the inspiratory reserve volume. The forced residual capacity (FRC) is the expiratory reserve volume plus the residual volume. Of course this capacity cannot actually be expired. The vital capacity (VC) is everything except the residual volume...that's why it's called "vital". The entire volume of air the lung can hold is the total lung capacity (TLC).